Beta-lactam antibiotic

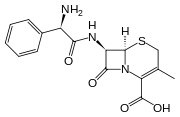
β-Lactam antibiotics are a broad class of antibiotics that include penicillin derivatives (penams), cephalosporins (cephems), monobactams, and carbapenems,[1] that is, any antibiotic agent that contains a β-lactam nucleus in its molecular structure. They work by attacking the cell walls of bacteria. They are the most widely used group of antibiotics.
Bacteria often develop resistance to β-lactam antibiotics by synthesizing Beta-lactamase, an enzyme that attacks the β-lactam ring. To overcome this resistance, β-lactam antibiotics are often given with β-lactamase inhibitors such as clavulanic acid.
Contents |
Clinical use
β-Lactam antibiotics are indicated for the prophylaxis and treatment of bacterial infections caused by susceptible organisms. At first, β-lactam antibiotics were mainly active only against Gram-positive bacteria, yet the recent development of broad-spectrum β-lactam antibiotics active against various Gram-negative organisms has increased their usefulness.
Mode of action
β-Lactam antibiotics are bactericidal, and act by inhibiting the synthesis of the peptidoglycan layer of bacterial cell walls. The peptidoglycan layer is important for cell wall structural integrity, especially in Gram-positive organisms. The final transpeptidation step in the synthesis of the peptidoglycan is facilitated by transpeptidases known as penicillin-binding proteins (PBPs).
β-Lactam antibiotics block not only the division of bacteria, including cyanobacteria, but also the division of cyanelles, the photosynthetic organelles of the glaucophytes, and the division of chloroplasts of bryophytes. In contrast, they have no effect on the plastids of the highly developed vascular plants. This is supporting the endosymbiotic theory and indicates an evolution of plastid division in land plants [2].
β-Lactam antibiotics are analogues of D-alanyl-D-alanine - the terminal amino acid residues on the precursor NAM/NAG-peptide subunits of the nascent peptidoglycan layer. The structural similarity between β-lactam antibiotics and D-alanyl-D-alanine facilitates their binding to the active site of penicillin-binding proteins (PBPs). The β-lactam nucleus of the molecule irreversibly binds to (acylates) the Ser403 residue of the PBP active site. This irreversible inhibition of the PBPs prevents the final crosslinking (transpeptidation) of the nascent peptidoglycan layer, disrupting cell wall synthesis.
Under normal circumstances, peptidoglycan precursors signal a reorganisation of the bacterial cell wall and, as a consequence, trigger the activation of autolytic cell wall hydrolases. Inhibition of cross-linkage by β-lactams causes a build-up of peptidoglycan precursors, which triggers the digestion of existing peptidoglycan by autolytic hydrolases without the production of new peptidoglycan. As a result, the bactericidal action of β-lactam antibiotics is further enhanced.
Modes of resistance
By definition, all β-lactam antibiotics have a β-lactam ring in their structure. The effectiveness of these antibiotics relies on their ability to reach the PBP intact and their ability to bind to the PBP. Hence, there are 2 main modes of bacterial resistance to β-lactams:
- Enzymatic hydrolysis of the β-lactam ring: If the bacterium produces the enzyme β-lactamase or the enzyme penicillinase, the enzyme will break open the β-lactam ring of the antibiotic, rendering the antibiotic ineffective. The genes encoding these enzymes may be inherently present on the bacterial chromosome or may be acquired via plasmid transfer, and β-lactamase gene expression may be induced by exposure to β-lactams. The production of a β-lactamase by a bacterium does not necessarily rule out all treatment options with β-lactam antibiotics. In some instances, β-lactam antibiotics may be co-administered with a β-lactamase inhibitor. However, in all cases where infection with β-lactamase-producing bacteria is suspected, the choice of a suitable β-lactam antibiotic should be carefully considered prior to treatment. In particular, choosing appropriate β-lactam antibiotic therapy is of upmost importance against organisms with inducible β-lactamase expression. If β-lactamase production is inducible, then failure to use the most appropriate β-lactam antibiotic therapy at the onset of treatment will result in induction of β-lactamase production, thereby making further efforts with other β-lactam antibiotics more difficult.
- Possession of altered penicillin-binding proteins: β-Lactams cannot bind as effectively to these altered PBPs, and, as a result, the β-lactams are less effective at disrupting cell wall synthesis. Notable examples of this mode of resistance include methicillin-resistant Staphylococcus aureus (MRSA) and penicillin-resistant Streptococcus pneumoniae. Altered PBPs do not necessarily rule out all treatment options with β-lactam antibiotics.
Nomenclature
β-Lactams are classified according to their core ring structures.
- β-Lactams fused to saturated five-membered rings:
- β-Lactams containing thiazolidine rings are named penams.
- β-Lactams containing pyrrolidine rings are named carbapenams.
- β-Lactams fused to oxazolidine rings are named oxapenams or clavams.
- β-Lactams fused to unsaturated five-membered rings:
- β-Lactams containing 2,3-dihydrothiazole rings are named penems.
- β-Lactams containing 2,3-dihydro-1H-pyrrole rings are named carbapenems.
- β-Lactams fused to unsaturated six-membered rings:
- β-Lactams containing 3,6-dihydro-2H-1,3-thiazine rings are named cephems.
- β-Lactams containing 1,2,3,4-tetrahydropyridine rings are named carbacephems.
- β-Lactams containing 3,6-dihydro-2H-1,3-oxazine rings are named oxacephems.
- β-Lactams not fused to any other ring are named monobactams.
Common β-lactam antibiotics
Penicillins (Penams)
Semisynthetic penicillins are prepared starting from the penicillin nucleus 6-APA.
Narrow-spectrum
- β-lactamase sensitive
- benzathine penicillin
- benzylpenicillin (penicillin G)
- phenoxymethylpenicillin (penicillin V)
- procaine penicillin
- Penicillinase-resistant penicillins
- methicillin
- oxacillin[3]
- nafcillin
- cloxacillin
- dicloxacillin
- flucloxacillin
- β-lactamase-resistant penicillins
- temocillin
Moderate-spectrum
- amoxicillin
- ampicillin
Broad-spectrum
- co-amoxiclav (amoxicillin+clavulanic acid)
Extended-spectrum
- azlocillin
- carbenicillin
- ticarcillin
- mezlocillin
- piperacillin
Cephalosporins (Cephems)
First generation
Moderate spectrum.
- cephalexin
- cephalothin
- cefazolin
Second generation
Moderate spectrum with anti-Haemophilus activity.
- cefaclor
- cefuroxime
- cefamandole
Second generation cephamycins
Moderate spectrum with anti-anaerobic activity.
- cefotetan
- cefoxitin
Third generation
Broad spectrum.
- ceftriaxone
- cefotaxime
- cefpodoxime
Broad spectrum with anti-Pseudomonas activity.
- ceftazidime
Fourth generation
Broad spectrum with enhanced activity against Gram positive bacteria and β-lactamase stability.
- cefepime
- cefpirome
Carbapenems and Penems

Broadest spectrum of β-lactam antibiotics.
- imipenem (with cilastatin)
- meropenem
- ertapenem
- faropenem
- doripenem
Monobactams
Unlike other β-lactams, the monobactam contains a nucleus with no fused ring attached. Thus, there is less probability of cross-sensitivity reactions.
- aztreonam (Azactam)
- tigemonam
- nocardicin A
- tabtoxinine-β-lactam
β-lactamase inhibitors
Although they exhibit negligible antimicrobial activity, they contain the β-lactam ring. Their sole purpose is to prevent the inactivation of β-lactam antibiotics by binding the β-lactamases, and, as such, they are co-administered with β-lactam antibiotics.
- clavulanic acid
- tazobactam
- sulbactam
Adverse effects
Adverse drug reactions
Common adverse drug reactions (ADRs) for the β-lactam antibiotics include diarrhea, nausea, rash, urticaria, superinfection (including candidiasis).[4]
Infrequent ADRs include fever, vomiting, erythema, dermatitis, angioedema, pseudomembranous colitis.[4]
Pain and inflammation at the injection site is also common for parenterally administered β-lactam antibiotics.
Allergy/hypersensitivity
Immunologically mediated adverse reactions to any β-lactam antibiotic may occur in up to 10% of patients receiving that agent (a small fraction of which are truly IgE-mediated allergic reactions, see amoxicillin rash). Anaphylaxis will occur in approximately 0.01% of patients.[4][5] There is perhaps a 5%-10% cross-sensitivity between penicillin-derivatives, cephalosporins, and carbapenems; but this figure has been challenged by various investigators.
Nevertheless, the risk of cross-reactivity is sufficient to warrant the contraindication of all β-lactam antibiotics in patients with a history of severe allergic reactions (urticaria, anaphylaxis, interstitial nephritis) to any β-lactam antibiotic.
Jarish Herxheimer reaction: Febrile reaction after first injection of penicillin in spirochetal infection, e.g., syphilis.
References
- ↑ Holten KB, Onusko EM (August 2000). "Appropriate prescribing of oral beta-lactam antibiotics". American family physician 62 (3): 611–20. PMID 10950216. http://www.aafp.org/afp/20000801/611.html.
- ↑ Britta Kasten und Ralf Reski (1997): β-lactam antibiotics inhibit chloroplast division in a moss (Physcomitrella patens) but not in tomato (Lycopersicon esculentum). Journal of Plant Physiology 150, 137-140 [1]
- ↑ "Mayo Clinic Proceedings". http://www.mayoclinicproceedings.com/inside.asp?AID=2547. Retrieved 2008-12-26.
- ↑ 4.0 4.1 4.2 Rossi S (Ed.) (2004). Australian Medicines Handbook 2004. Adelaide: Australian Medicines Handbook. ISBN 0-9578521-4-2.
- ↑ Pichichero ME (April 2005). "A review of evidence supporting the American Academy of Pediatrics recommendation for prescribing cephalosporin antibiotics for penicillin-allergic patients". Pediatrics 115 (4): 1048–57. doi:10.1542/peds.2004-1276. PMID 15805383. PMID 15805383
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||